Many articles over the past several months have focused on the damage stress has had on our bodies during the COVID pandemic. These articles state stress, anxiety, isolation, and depression are key emotional issues developed as a result of COVID-19. Here are some of the things the articles have stated:
Joseph McGuire, PhD, MA, child psychologist with Johns Hopkins Medicine
Stressed About COVID-19? Here’s What Can Help | Johns Hopkins Medicine
Stress can affect the immune system, but it is uncertain whether short-term stress makes someone more likely to catch the new coronavirus, says McGuire. Taking steps to reduce your stress in a healthy way is important.
Lois Parshley is a freelance investigative journalist, Sept 3, 2020
Covid-19 risk factors: How chronic stress and the coronavirus might be linked – Vox
2020 has been remarkably stressful — from the fear of nuclear war to a presidential impeachment to a pandemic that has killed more than 482,500 people in the U.S. alone.
KFF (Kaiser Family Foundation) Tracking Poll gave the following statistics in January, 2021
The Implications of COVID-19 for Mental Health and Substance Use | KFF
January 2021, about 4 in 10 adults in the U.S. have reported symptoms of anxiety or depressive disorder, a share that has been largely consistent, up from one in ten adults who reported these symptoms from January to June 2019.
Households experiencing income or job loss (53%) are significantly more likely than households that haven’t had job loss (32%) to report that worry or stress over the coronavirus outbreak has negatively impacted their mental health.
Non-Hispanic Black adults (48%) and Hispanic or Latino adults (46%) are more likely to report symptoms of anxiety and/or depressive disorder than Non-Hispanic White adults (41%).
We have heard that underlying conditions of chronic diseases such as cancer, type II diabetes, and obesity significantly contribute to the worsening of infections and the number of deaths we have seen due to COVID-19. But we also hear that children and adults without these types of underlying conditions have had severe infections and died from COVID also. Could it be that chronic distress is the underlying condition impacting the severity of COVID-19?
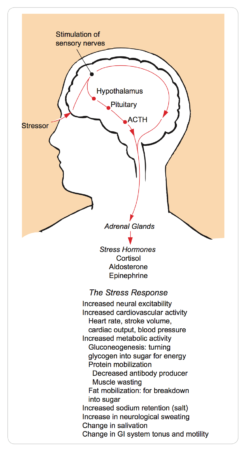
The answer is “yes.” Distress can be considered an underlying condition. A chronic disease is the outward condition of an out of control distress on the body. The human body is designed to handle perceived or real stress with several backup mechanisms to help ensure physical survival. Two different body systems, nervous and endocrine, are called upon depending on how prolonged the stress is on the body.
Here’s how the systems work:
Whenever we feel or perceive danger is near us – the nervous system responds with a fight or flight stress response – it releases epinephrine and norepinephrine to produce the energy we need. This is an immediate solution to get us through a short term or acute danger (2-3 seconds). Depending on how long the danger persists, the nervous system will relinquish its role to the endocrine system which can handle the danger for a few minutes to a prolonged period of time. The endocrine system will release cortisol from the adrenal medulla gland for a few minutes and then from the neuroendocrine pathways (ACTH, vasopressin, and thyroxin) for the prolonged time to help with survival. ACTH increases cortisol release, vasopressin increases water reabsorption and decreases perspiration in the body, and thyroxin increases metabolism.
All of this is to say, a prolonged distress response by the systems has a lasting harmful effect on the bodies’ organs including the brain, kidneys, heart, and thyroid and the immune system. Whether a physician has already identified the disease caused by the prolonged stress and inflammation of the body, i.e., arthritis, cancer, heart disease, obesity, type II diabetes, or the prolonged distress is causing internal issues that are not yet seen physically, the immune system is compromised. As a result, whether it be COVID or any other illness, the body will have a difficult time fighting it.
What we know about COVID 19 and cortisol levels:
Covid-19 risk factors: How chronic stress and the coronavirus might be linked – Vox
New research suggests cortisol levels appear to impact the severity of COVID-19. There’s still a lot we don’t understand about the relationship of the two, but clinical trials using dexamethasone have reduced the body’s natural cortisol production as well as inflammation in the body and been found to help critically ill patients.
“High levels of cortisol are associated with poor [Covid-19] outcomes, and drugs that block the hormone seem to improve outcomes,” says Kavita Vedhara, a University of Nottingham professor of health psychology who conducted a study on Covid-19 and stress. Vedhara says while further research is needed, she wouldn’t be surprised if chronic stress was found to be a risk factor for a severe case of Covid-19. “It fits with what we know about psychological stress generally, and in particular the evidence on stress and other viral infections,” she added.
Our ability to manage stress on a daily basis is important to surviving any illness that might come our way. Look for my next blog on how to minimize distress (bad stress) and enhance eustress (good stress). In the meantime, here are some tips for coping with negative emotions you may experience.
National Institute of Mental Health: This group has focused on coping with negative emotions
NIMH » Shareable Resources on Coping with COVID-19 (nih.gov)